Do you feel supported in your journey with diabetes?
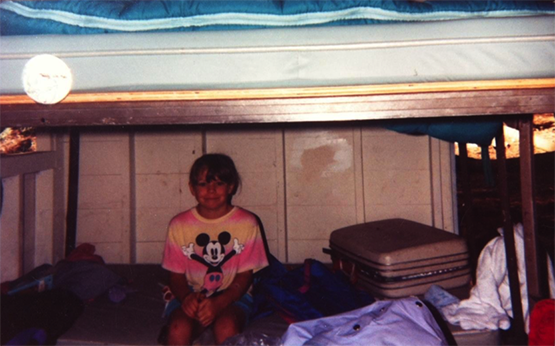
I feel very supported in my journey with diabetes. My mom forced me to go to diabetes camp the first year and she was so nervous that I would hate it. She says I cried when I came back because I didn’t want to leave – I was 8 years old. I learned early on the importance of community.
What do you think is the most important thing people should understand about diabetes?
Diabetes is a full-time job that you didn’t apply for, don’t want, and can’t quit. There is no vacation and no pay. I think understanding the impact that diabetes has can help to understand why there is no “perfect” diabetes management and how moods and attitude can vary with blood sugar change in people with diabetes. The biggest challenge diabetes poses for me is that it can be so interruptive. Right when you think you’ve got a pattern figured out, then BAM, something changes.
What is the biggest change you’ve seen in yourself since your diagnosis?
By nature, I am not an organized planner, I like adventure and spontaneity, and even impulsivity. Diabetes has balanced this and calmed me down in a significant way. I get direct feedback from my body about how to slow down and be present.

When did you decide to go into nursing?
In my third year of undergraduate studies, I knew that helping people with diabetes had to be in my future, at that point I thought that I would be an endocrinologist. With more studying, I realized my passion was in helping people understand the disease and cope with it, not so much in studying the disease itself. I changed my career path to nursing, and have loved that choice, it is a great fit for me.
What do your colleagues at work know about your diabetes?
My colleagues at work consider me a diabetes expert. I am very open with them about it, and try to help them understand it as much as possible. I am open with my blood sugars and I think that has helped them to let go of the idea of perfect control and to judge our patients’ challenges less.
How do you manage your diabetes around your work schedule?
I have a much more regular schedule now than I did when I started out. I work three 12-hour shifts in two weeks and the rest is flexible office time. On my office days, life is a lot easier with diabetes - I am able to exercise and eat responsibly. During my 12-hour shifts I have less flexibility so the stakes are higher with diabetes management. Having a continuous glucose monitor (CGM) to give me feedback about my patterns has helped a lot.
The most interesting pattern I noticed is that I tended to go low in the late afternoon on 12-hour work days - I think it was related to lower stress at the end of a shift, so I created a personal basal profile to meet my insulin needs on those days. I have very few lows since using the profile.
Do you ever have trouble remembering to take care of yourself when you’re doing so much for others?
Yes, most definitely. To hold me accountable to my own BGs, I set my alarms a little tighter at work so that I do not put my patients at risk by not paying attention to myself. I think being a nurse helps me to better care for my diabetes because I am so dependent on my brain working optimally on a minute to minute basis – this keeps me more in touch with the state of my blood sugar than sitting at home watching TV.
Can you give an example of a time when your own diabetes was an asset when you were caring for a patient?
There are too many times to count. The patients themselves are usually too stressed or tired for me to make a big impact, so it’s usually the parents who benefit the most from learning that I have thrived with diabetes for 25 years.

Have you always used an insulin pump? If not, what aspects of pump therapy were appealing to you when you made the switch?
I switched to an insulin pump when I was 15 years old. I was using NPH and Humalog and struggling to manage playing soccer and changing daytime routines. I remember crying when the pump trainer was at my house and not understanding why. Now, looking back after my experiences with my patients, I know that making such a big change in a daily routine can be very scary. I needed to learn to trust my new routine.
The flexibility my pump gives me for real-time blood sugar management has been so helpful in understanding my diabetes better and as a result reducing the interruptions in my life.
How did you hear about insulin pumps by Tandem Diabetes Care?
I first saw a Tandem pump when my good friend got one. I thought she was brave to try a new pump company and I saw her so happy with the pump. I remember how impressed I was with how modern the technology looked and felt - something I didn’t see in my previous pump.
What recommendations do you have for anyone newly diagnosed with diabetes?
There is nothing like having people who understand the intricacies of what it is like to experience diabetes, the ups, downs, frustrations, successes. To anyone with diabetes, I recommend that you find your people and see them often. Work hard to find a healthcare provider that suits you. You need to feel comfortable to ask questions and get answers you feel are respectful and constructive answers.
From time to time, we may pass along: suggestions, tips, or information about other Tandem Insulin Pump user experiences or approaches to the management of diabetes. However, please note individual symptoms, situations, circumstances and results may vary. Please consult your physician or qualified health care provider regarding your condition and appropriate medical treatment. Please read the Important Safety Information linked below before using a Tandem Diabetes Care product.