It’s time for a vacation to somewhere exciting!
Or maybe you just have a work trip for a few days (hopefully there’s time to do something fun, too).
Maybe you’re flying to your next destination, or maybe you’re going on a road trip. No matter what, you are going to be thrown off your normal routine, which will require a little extra thought during the planning process to provide you with peace of mind around your diabetes
… and ensure the trip is as amazing as possible.
Without further ado, here are some things to consider for your next trip:
1. If you’re flying, prepare to assist TSA.
Your device is safe for use during air travel and complies with FAA wireless transmission standards. It is also designed to withstand common electromagnetic interference and can be safely carried through metal detectors.
Some TSA agents are more knowledgeable than others. You can help by knowing your pump’s needs. Before you go, be sure to review Tandem Diabetes Care’s screening recommendations and access their air-travel note that you can carry with you and share with the TSA or airport representative.
2. Have low snacks WITH you at your seat.
I can already hear it.
“Well, if my blood sugar goes low, the flight attendant can just get me some juice or some soda, and I’ll be fine.”
Sure, that could be the case, but what happens if your blood sugar goes low during takeoff or landing, when the flight attendants must be seated? Or if there is an extended period of turbulence, and they’re unable to get you a sugary beverage?
I’ve had a similar conversation with people who say, “I have a dollar on me. If I go low, I’ll find something at a vending machine.” When you get down to it, you can’t eat the dollar to help your blood sugar.
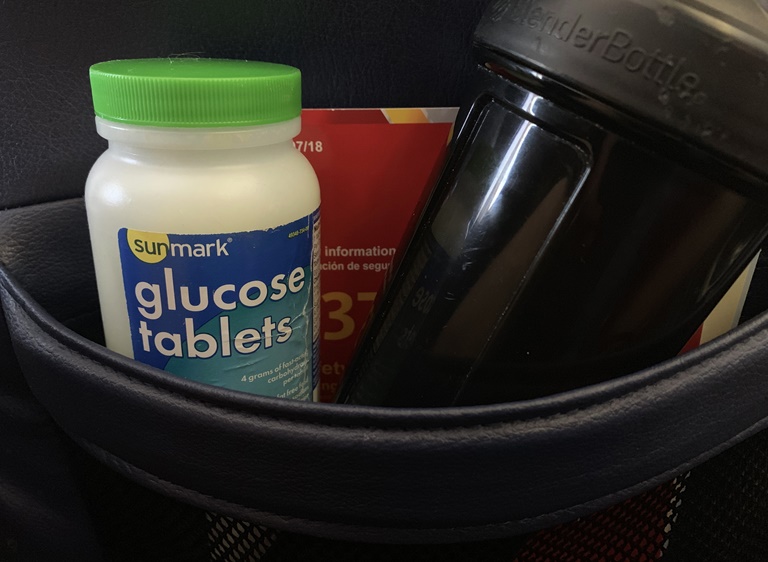
Have glucose tabs, a granola bar, regular soda, or SOMETHING that can raise your blood sugar at the very least, in the bag underneath your seat.
3. When flying or driving, consider a temporary basal rate.
Pop Quiz: What do a long flight and a day-long car ride have in common besides transporting you from one place to another?
If you answered, “Extended periods of inactivity” or “Lots of sitting,” you win!
Yes, unfortunately, on a plane or in a car, there’s not much of a chance to move.
When one moves less than normal, the body doesn’t respond in the nicest way. In fact, it tends to respond in the form of higher blood glucose.
This can also lead to dehydration. These two are more related than you may realize.
When you fall short on fluids, the blood glucose in circulation becomes more concentrated, and high blood sugar can cause you to urinate more, which results in even more dehydration.
Throw in the fact that if you are flying, the altitude and conditioned air also dehydrate you. It’s a vicious cycle, and not one you want to be part of.
This is where a temporary basal increase could pay HUGE dividends for helping maintain blood sugar in the target range.
Setting that temporary basal for the duration of your transportation may be a great start.
The amount of insulin required depends on your unique needs. It’s important to talk to your healthcare provider to go over your travel plans.
4. Extended boluses may be your best friend at restaurants.
Eating is one of the many awesome things about traveling, especially when you travel to an area that is well known for its food (think: NYC, New Orleans, etc.).
If you visit a restaurant where the food is high in fat and carbs, you may experience stubborn high blood sugars hours after the fact.
Enter: The Extended Bolus feature. (That's an earlier blog I wrote about it.)
Is it easy to be perfect? No. Should you still make smart choices when eating away from home and try to stay on your nutrition plan? Of course.
Should you also enjoy the cuisine around you? Absolutely.
5. Try to squeeze in some form of exercise.
Exercise can help with your insulin sensitivity. If you are on an extended trip and do NOT exercise as much as you usually do, you may notice your blood sugars start to trend higher than you’d like.
The major keys here are going to be prioritizing and being creative when need be. It is SUPER easy to throw exercise to the wayside and just “relax,” but sticking to your usual routine as well as possible will pay off in the long run.
Staying at a hotel? It likely has some sort of gym with basic cardio equipment and weights. Not staying at a hotel? Remember you can be active outside or do a body-weight workout.
There are ways around everything if you want it enough.
6. Pack 2-3 times the insulin pump supplies you think you’ll need.
If you expect to do two site changes during your trip, bring enough supplies for six.
If you expect to do four site changes, bring enough supplies for 10.
This may seem excessive, but as we all know, the key to thriving with diabetes is to expect the unexpected.
If your site fails, falls off, or is ripped out by accident prior to your trip being completed, having double to triple the amount of supplies means you won’t have to worry about a transition to injections for a few days. You should always bring backup insulin just in case you get separated from your pump supplies.
“Well Ben, wouldn’t eight be a LOT of infusion sets to have when I only anticipate four site changes?”
Sure it is, but have you ever had a time where you’ve gone through three sets in a day due to fluky circumstances? It’s uncommon, but I have in my 16 years of being on a pump.
It is better to be over-prepared than under-prepared when you are away from home and away from your stash of supplies so you don’t find yourself calling the (amazing) Tandem support team in the middle of the night from a city halfway across the country because you don’t have enough sets to do a site change.
Oh, and Tandem offers a traveler loaner program for additional peace of mind. If you will be traveling to areas outside of the US (or Canada if you live there) or where you can’t easily receive shipments, you can take a second pump with you. For more information, give them a call at (877) 801-6901.
Implementing these tips and tricks should help your mind be at ease, keep you prepared, and have you ready to enjoy your next trip to the fullest!
More on the blog: Travel Easily with Tips from Kerri Sparling!
Author Bio: Ben Tzeel has lived with type 1 diabetes since 1999. He has a master’s degree in nutrition from the University of North Carolina at Chapel Hill and is a registered dietitian. He is a Certified Strength and Conditioning Specialist (CSCS) through the National Strength and Conditioning Association, is a published fitness model, and writes about exercise and nutrition.
Ben Tzeel was compensated by Tandem Diabetes Care for his contribution on this topic. However, he created the content and it is based on his personal knowledge, experiences, and observations.
From time to time, we may pass along: suggestions, tips, or information about other Tandem Insulin Pump user experiences or approaches to the management of diabetes. However, please note individual symptoms, situations, circumstances and results may vary. Please consult your physician or qualified health care provider regarding your condition and appropriate medical treatment. Please read the Important Safety Information linked below before using a Tandem Diabetes Care product.