Medically reviewed by Dr. Jordan Pinsker, MD, Chief Medical Officer, Leah Fuller McLane, PharmD, BC-ADM, CDCES, and Amy Rich, DNP, CRNP-BC, CDCES, Medical Science Liaisons with Tandem Diabetes Care.
Ketones are a natural by-product of the body breaking down its backup energy source — fats — during a process called ketosis.
For a person living with diabetes, ketones can pose a significant risk to overall health. While ketones occur naturally, too many can trigger diabetic ketoacidosis (DKA), a life-threatening condition that should be diagnosed and treated immediately. It’s important for someone living with diabetes to understand what ketones are, how to prevent or reverse the buildup of ketones in the bloodstream, and how to identify the symptoms of DKA.
What are Ketones?
Understanding Ketones
“Ketones are acids that are produced when the body breaks down fat instead of glucose for energy, and they can build up in the blood and urine,” said Leah Fuller McLane, Senior Medical Science Liaison Manager at Tandem Diabetes Care.
This breakdown of fats occurs naturally as a result of carbohydrate deprivation, such as when you’ve been sleeping or fasting. Ketones accumulate in the bloodstream during this process, called ketosis, and are naturally excreted in the urine.
“Having some ketones in the urine or blood can be normal, but if there are too many, the body’s chemistry can become too acidic,” said McLane.
Ketoacidosis is the result of high acidity in the bloodstream due to ketones.
Insulin and ketones
A person with diabetes doesn’t naturally produce the hormone insulin, or they can't produce enough insulin to effectively convert the glucose in the food that they eat into energy. Insulin helps to process and reduce the level of glucose.
“Everyone needs insulin because it acts like a key that allows glucose to get into the body’s cells so it can be used as energy,” said Fuller McLane. “When the body does not have enough insulin or glucose, other molecules start to break down.”
Most people produce insulin naturally in an abdominal gland organ called the pancreas. For people living with type 1 diabetes (T1D), insulin must be manually introduced into the body via an injection, insulin pump infusion, or inhaler. As a result, a person with T1D is at a higher risk of DKA and possible life-threatening complications.
Detecting Ketones
A simple blood or urine test is used to determine the level of ketones present in the body.
A small fingerstick blood sample can be used with an electronic meter to determine if the level of ketones in the bloodstream is too high.
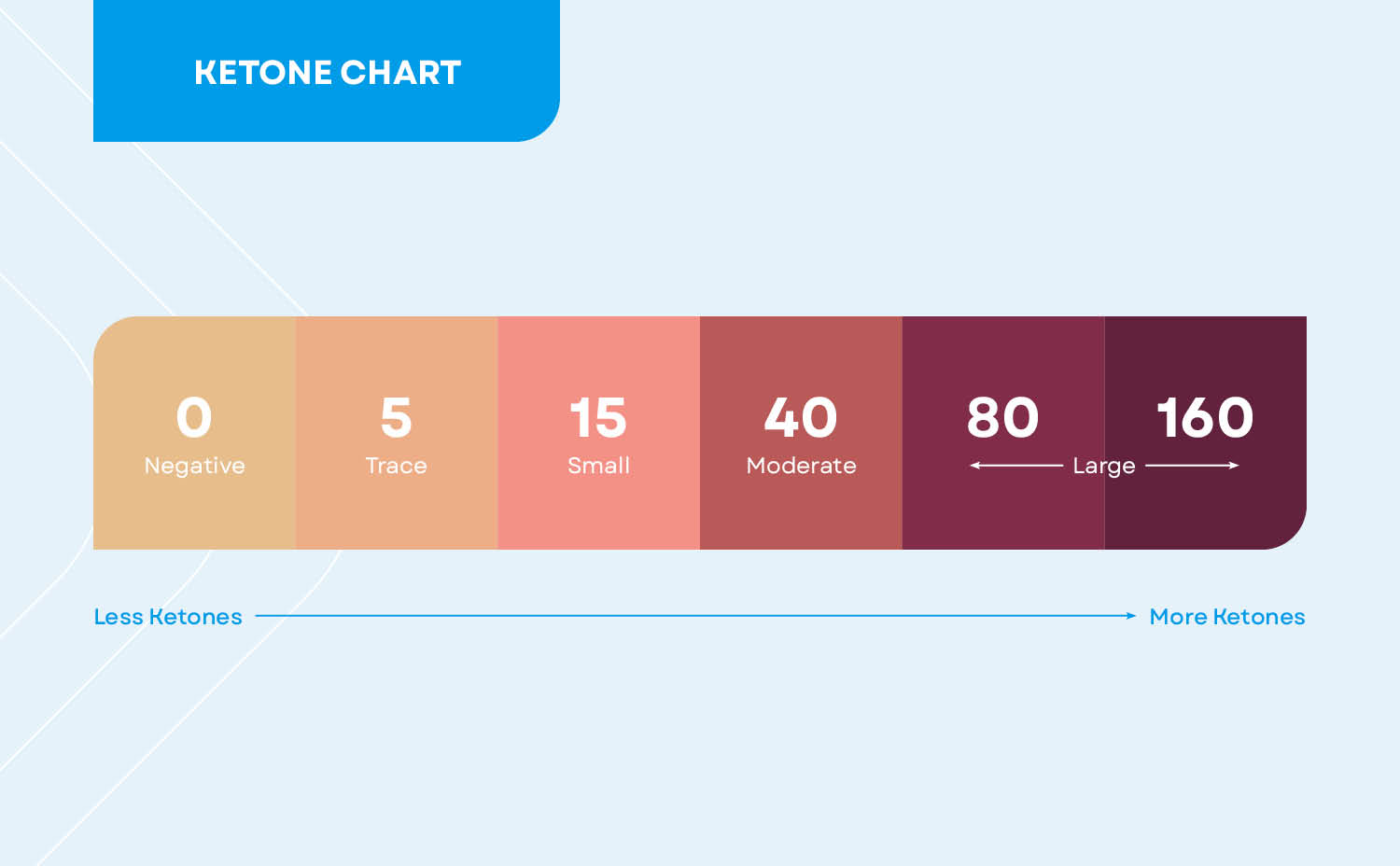
Urinalysis ketone test strips are a more common form of ketone testing and are available over the counter at pharmacies or with a prescription. With this method, a color-changing test strip is dipped into a urine sample to detect the presence of ketones.
Be sure to carefully read the instructions on the product label to correctly test for the presence of ketones. Most brands of ketone urinalysis test strips have a color-coded scale on the strip bottle to help determine the approximate level of ketones present. A darker color on the test strip will indicate a higher level of ketones in the urine sample and a higher risk of ketoacidosis.
When to test for ketones
Always consult with a healthcare professional to discuss when you should test for ketones and what steps to take if you find you have ketones present in your blood or urine.
It is recommended that people living with diabetes keep urinalysis ketone test strips on hand. Test for ketones if you have any symptoms of high blood sugar or DKA, or in times of increased risk (see below). If ketones are detected, it is recommended that the person contacts their doctor right away.
People living with T1D should test for ketones if they:
- Had a recent injury or illness, especially if they are vomiting, dehydrated, or are having difficulty eating
- Have blood sugars that are persistently high and not responding to therapy (greater than 250 mg/dL or at the level indicated by their doctor)
- Are experiencing symptoms of DKA
- Experienced an interruption in insulin delivery (missed doses, infusion set occlusions, pump failure, etc.)
If any of these situations apply, test every few hours until the situation has resolved.
“It is important for people to discuss ketone findings with their healthcare providers to discuss their specific care plan,” said Amy Rich, Medical Science Liaison at Tandem Diabetes Care. “If there are small or trace amounts of ketones, monitor blood sugar levels closely and increase fluid intake.Test for ketones again in a few hours.If the patient is unable to reach their provider and they have elevated glucose levels, moderate or high ketones, and are symptomatic, it is important that they are evaluated in an emergency room.”
Your doctor may recommend testing for ketones at additional times, such as during pregnancy, when starting new medications, or during periods of high stress.
What it means to have ketones
If an elevated level of ketones is found in a urine or blood sample, the level of ketones in the bloodstream is too high. This can indicate a high risk of ketoacidosis.
Ketones often accompany high blood sugars in people with diabetes, but this isn’t always the case.
“Some medications for diabetes can decrease the need for insulin while keeping blood sugars at a normal level, so the presence of ketones could be concerning before glucose levels are elevated,” said Fuller McLane. “It is important for people with diabetes to work with their doctors to develop an individualized plan on how to handle any level of ketones.”
In addition to diabetes, other factors that increase the risk for elevated ketone levels include pregnancy, a low-carbohydrate diet, certain medications, excessive alcohol intake, or dehydration. Consult your physician if you find that you have ketones in your urine and have one or more of these risk factors.
Symptoms of Ketone Accumulation
Common symptoms of Ketoacidosis
Early symptoms of high ketone levels are similar to symptoms of high blood sugar levels, so it is important to check ketone and glucose levels if you are experiencing these symptoms.
Symptoms of elevated ketone levels may include:
- Extreme thirst
- Dry mouth
- Frequent urination
- Headache
- Fatigue
- Nausea
- Stomach Pain
- Vomiting
If you experience these symptoms and ketone or glucose levels are elevated, call your healthcare provider. If your healthcare provider is unavailable and you are at a higher risk of DKA, it is recommended that you visit an emergency room to be evaluated.

Recognizing the signs of diabetic ketoacidosis (DKA)
If ketone levels stay elevated or continue to rise in a person with T1D, the condition can worsen and the person could go into DKA within hours.
Symptoms of DKA may include:
- Fruity-smelling breath
- Dry or flushed skin
- Nausea
- Vomiting and/or stomach pain
- Difficulty breathing
- Cognition changes or confusion
DKA can be deadly if left untreated. If a person with diabetes is experiencing symptoms of DKA, it is important to seek medical attention. If their physician is unavailable, seek emergency care.
See our article on Diabetic Ketoacidosis in Juveniles for more information on how to recognize and combat DKA in kids and teens.
Managing and Preventing Ketones
Strategies to prevent elevated ketone levels
Ketones occur naturally, and trace amounts of ketones in urine for people without diabetes is rarely cause for alarm. There are several reasons why a person without diabetes may experience ketones in their urine, including excessive alcohol intake, following a low carb diet, dehydration, or pregnancy. However, higher levels of ketones could indicate an underlying problem. Talk to your doctor if you do not have diabetes and are concerned about ketones in your urine.
For those living with diabetes, and especially for those living with T1D, prevention is the best strategy for reducing ketone levels.
Prevention methods include:
- Practicing proper insulin management and storage, such as following the insulin therapy plan you and your doctor agree on and storing unopened insulin in a cool place without freezing
- Maintaining adequate hydration
- Following a balanced, nutritional diet or T1D meal plan
Exercise is part of a healthy lifestyle and can help long-term glucose level management. However, people living with T1D should consult with a doctor regarding exercise while ketones are present. Exercise may adversely affect the presence of ketones if blood sugar levels exceed 250 mg/dL.
In addition, use of an advanced hybrid closed-loop (AHCL) system, such as Control-IQ technology available in insulin pumps from Tandem Diabetes Care, is associated with a lower rate of DKA than historical data.1 Control-IQ technology uses CGM values* to predict and help prevent highs and lows up to 30 minutes in advance. Learn more about Control-IQ technology on our website.
Unless otherwise noted, all medical information was provided by Leah Fuller McLane, PharmD, BC-ADM, CDCES, and Amy Rich, Medical Science Liaison of Tandem Diabetes Care, Inc, and reviewed by Dr.Jordan Pinsker, MD, Chief Medical Officer with Tandem Diabetes Care.
Responsible Use of Control-IQ Technology: Control-IQ technology does not prevent all highs and lows. You must still bolus for meals and actively manage your diabetes. Please visit tandemdiabetes.com/responsible-use for more information.
* CGM sold separately.
Reference: 1. Graham R, Mueller L, Manning M, et al. Real-World Use of Control-IQ Technology is Associated with a Lower Rate of Severe Hypoglycemia and Diabetic Ketoacidosis than Historical Data: Results of the Control-IQ Observational (CLIO) Prospective Study. Diabetes Technol Ther. 2024;26(1):24-32. doi: 10.1089/dia.2023.0341.
Important Safety Information
RX ONLY.
Indications for Use:
Tandem Mobi system: The Tandem Mobi insulin pump with interoperable technology (the pump) is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in persons requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is intended for single patient, home use and requires a prescription. The pump is indicated for use in individuals 6 years of age and greater.
t:slim X2 insulin pump: The t:slim X2 insulin pump with interoperable technology is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in people requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is intended for single patient use. The pump is indicated for use with NovoLog or Humalog U-100 insulin. The pump is indicated for use in individuals 6 years of age and greater.
Control-IQ technology: Control-IQ technology is intended for use with compatible integrated continuous glucose monitors (iCGM, sold separately) and alternate controller enabled (ACE) pumps to automatically increase, decrease, and suspend delivery of basal insulin based on iCGM readings and predicted glucose values. It can also deliver correction boluses when the glucose value is predicted to exceed a predefined threshold. Control-IQ technology is intended for the management of Type 1 diabetes mellitus in persons 6 years of age and greater. Control-IQ technology is intended for single patient use. Control-IQ technology is indicated for use with NovoLog or Humalog U-100 insulin.
Warning: Control-IQ technology should not be used by anyone under the age of 6 years old. It should also not be used in patients who require less than 10 units of insulin per day or who weigh less than 55 pounds.
Control-IQ technology is not indicated for use in pregnant women, people on dialysis, or critically ill patients. Do not use Control-IQ technology if using hydroxyurea. Users of a Tandem insulin pump and Control-IQ technology must use the insulin pump, CGM, and all other system components in accordance with their respective instructions for use; test blood glucose levels as recommended by their healthcare provider; demonstrate adequate carb-counting skills; maintain sufficient diabetes self-care skills; see healthcare provider(s) regularly; and have adequate vision and/or hearing to recognize all functions of the pump, including alerts, alarms, and reminders. The Tandem pump and the CGM transmitter and sensor must be removed before MRI, CT, or diathermy treatment. Visit tandemdiabetes.com/safetyinfo for additional important safety information.