Medically reviewed by Dr. Jordan Pinsker, Vice President & Medical Director, Tandem Diabetes Care.
Diabetic ketoacidosis (DKA) is a serious complication of type 1 diabetes, and, less commonly, type 2 diabetes. In newly diagnosed cases of type 1 diabetes, DKA is often the point of diagnosis for individuals who have been symptomatic and unwell. Untreated, diabetic ketoacidosis can lead to serious consequences, potentially even death.
DKA typically gets treated urgently through emergency rooms and hospital admissions. It’s important for someone living with diabetes, or their caregiver, to know the signs of diabetic ketoacidosis, when to seek treatment, and when someone may be experiencing it for the first time.
To understand the signs of DKA, it is important to first understand some basics of diabetes. Type 1 diabetes is an autoimmune disease where the body attacks the cells in the pancreas responsible for producing insulin. Because of this attack, the cells are not able to produce insulin.
Insulin is like a key that opens the door to the parts of your body that need to use glucose for energy. When your muscles need glucose for energy, insulin allows them to absorb that glucose. When your brain is thinking and using energy, insulin allows your brain to absorb glucose from the bloodstream.
When insulin is not there, the body will turn to other sources of fuel for nourishment, such as fat. This can quickly become a medical emergency.
What is Diabetic Ketoacidosis?
During this medical emergency, when the body either does not have enough insulin, or is not able to use the insulin that is there (perhaps due to an illness, like the flu), it tries to use an alternative fuel source, such as breaking down fat. This very quickly causes a problem, because breaking down fat leads to the creation of something called ketones.
Ketones can make the blood acidic, which in turn can lead to diabetic ketoacidosis. During this process a person may feel very fatigued, may experience vomiting, or may experience severe cramps particularly in the stomach. There may also be excessive thirst and frequent urination.
Note: This is not the complete list of symptoms of diabetic ketoacidosis and may not reflect DKA in all individuals. See below for a more extensive list of possible symptoms of DKA.
Here is an explanation from Dr. Jordan Pinsker, Vice President and Medical Director of Tandem Diabetes Care, who is a leading pediatric endocrinologist:
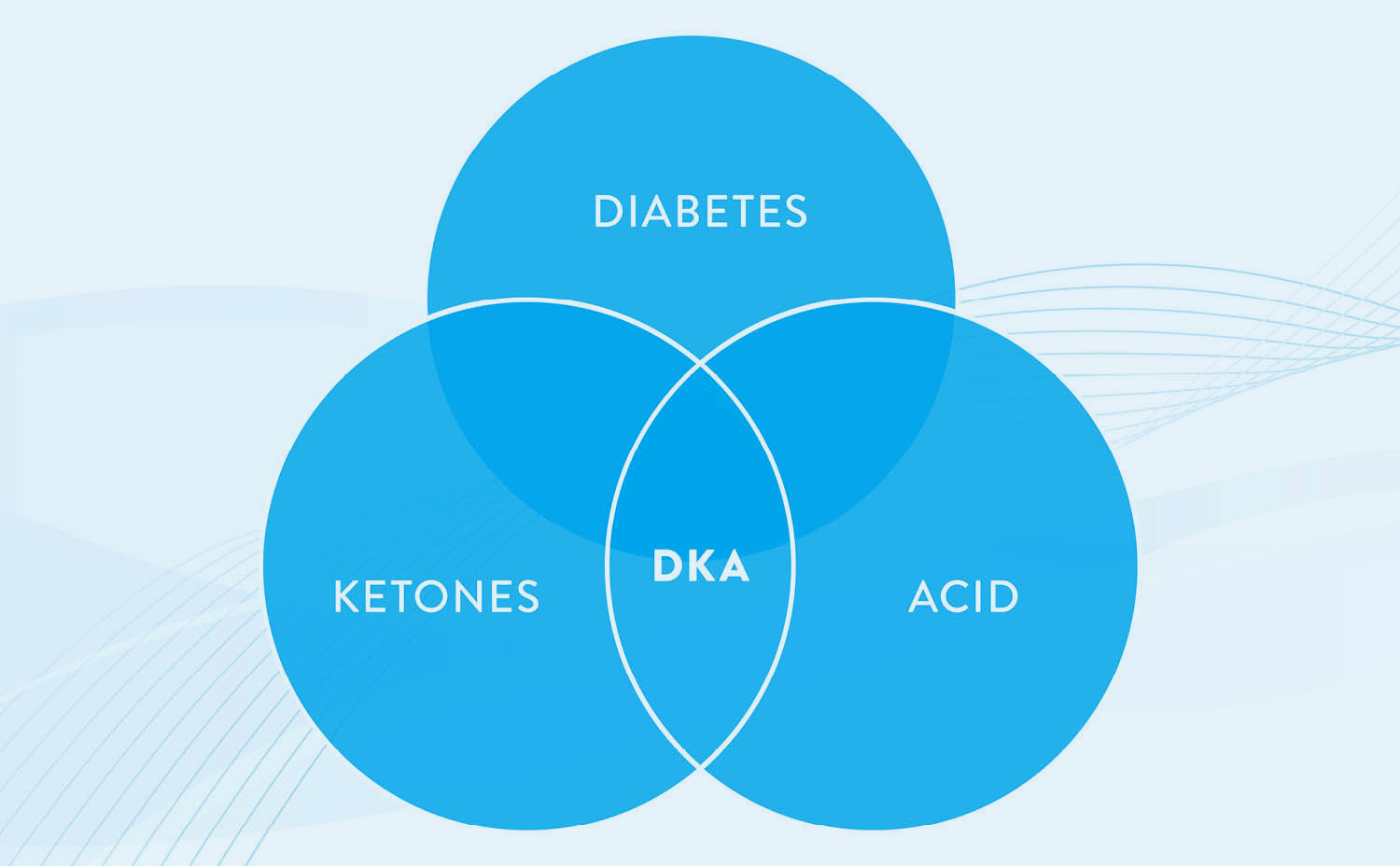
“Here’s how I describe diabetic ketoacidosis to my patients. DKA stands for diabetes, ketones, and acid. Everyone who has been diagnosed with type 1 diabetes already has the ‘D.’ You already have diabetes and you’re taking insulin to control blood sugars. When first diagnosed, when your body is resistant to insulin, or if you forget to take insulin or you don’t take enough insulin, you can’t absorb all of the glucose in the blood, so your body has to break down fat as another source of energy.
That’s only good for a short amount of time to serve as an alternate energy source. The problem with this is that ketones — a byproduct of using this alternative fuel source — can quickly make you quite sick. They turn your blood to acid. So, ketones are an early warning sign that you’re getting sick. You always have the ‘D.’ The ‘K’ in the middle stands for ‘ketones’ and serves as a warning sign that things aren’t going so well, and you don’t want to get to the ‘A’ part.”
With a firmer understanding of diabetic ketoacidosis, it’s time to examine the signs of diabetic ketoacidosis.

What are the Signs of Diabetic Ketoacidosis?
The two most critical signs of diabetic ketoacidosis are vomiting and stomach pain, said Dr. Pinsker.
“With repeated high blood sugars that won’t come down, or belly pain, you have to make that first assumption that you have ketones and you’re in diabetic ketoacidosis,” he explained. “You have the ‘D’ already and you might now have the ‘K’ part with these symptoms, but you can turn it around before you get to the ‘A’ part. You need to take extra insulin, check your infusion site if using an insulin pump, and stay well hydrated by drinking a lot of water. That is why checking for ketones can be really helpful.
“But sometimes things happen. If you are vomiting or have other severe symptoms, you need to go to the emergency room. There you can get fluids and more insulin, and in many cases need to be admitted to the hospital.
“Spell it out. That’s how I teach it. As soon as you’ve got ‘K,’ we’ve got work to do to try to prevent getting to the ‘A.’”
While vomiting and stomach pain might be two major signs of diabetic ketoacidosis, there are still other possible symptoms to be aware of.
Note: The following symptoms may not be an indication of diabetic ketoacidosis for all individuals. Please consult a healthcare professional for further information.
Additional symptoms of diabetic ketoacidosis could include:
- Excessive thirst
- Frequent urination
- Nausea
- Confusion
- Fatigue
- Shortness of breath
- Irritability
- Dry mouth or eyes
- Fruity-scented breath
- Rapid breathing
What are the Signs of Diabetic Ketoacidosis in Children and Teenagers?
The signs of diabetic ketoacidosis in children, adolescents, and teenagers are the same as in adults. Someone who has type 1 diabetes, or someone with insulin dependent type 2 diabetes, regardless of age, should act immediately if they are experiencing the above symptoms — with special attention being given to nausea, vomiting, and stomach pain.
A caregiver or parent of a child with type 1 diabetes should be aware of the symptoms of diabetic ketoacidosis.

Have a DKA Plan in Place
Someone living with type 1 diabetes should already have a customized plan in place that they’ve outlined with their healthcare professional. If they haven’t, it is recommended by Dr. Pinsker that they speak with their doctor.
“You should have a DKA management plan that has been discussed and defined by your doctor,” Pinsker said. “You should have a hyperglycemia ketone plan of how you’re going to give extra insulin and how much water you’re going to drink, and when you’re going to call if you have ketones.
“Also, if you are using an insulin pump, you need to have a plan of when to give a backup injection of insulin so you know it went in, then change out your pump site. Ketones are often a sign you don’t have enough insulin, which could mean the insulin is not going into your body, so you might need to change out the pump site for insulin pump users. There’s no point in measuring ketones if you’re not going to do anything. You have to react while you’re still at the ‘K’ so we can do something about it.”
Treating Ketoacidosis in Children and Teenagers
At the earliest signs of diabetic ketoacidosis, it is recommended that you test your ketones at home. This can be done through either a urine test strip or a blood ketone meter as an early-warning system. Consistently checking and understanding blood glucose levels can help. You may need to ask your doctor for a prescription for ketone test strips to have on hand.
However, because type 1 diabetes can be unpredictable, understanding when it’s time to seek medical attention is critical.
“If you’re vomiting, you can’t keep any food or liquid down, and your blood sugar will not go down, you need to go in (to get medical treatment),” Dr. Pinsker said. “Hydration through an IV will help. You can even get insulin through an IV. While it’s uncommon, diabetic ketoacidosis can be fatal. It occasionally happens so we don’t want to be messing around. Once you’re symptomatic, you need to go to a doctor and get treatment.”
Remember the D-K-As of diabetic ketoacidosis. If you have diabetes, you’ll work to prevent ketones, and if you have ketones you need to have a plan in place with your doctor on the steps you will take to avoid the acidosis. With D, you’ll need to prevent the K or turn it around, to avoid the A.
Learn More About Insulin Pumps
Tandem Diabetes Care is committed to improving the lives of people living with diabetes. The t:slim X2 insulin pump with Control-IQ technology is cleared for type 1 diabetes insulin therapy for children as young as 6 and can anticipate glucose levels 30 minutes in advance and automatically adjust dosing. That means more time in range,* and more protection from highs and lows.
Unless otherwise noted, all medical information was provided by Jordan Pinsker, MD, and Molly McElwee Malloy, RN, CDCES of Tandem Diabetes Care, Inc.
Responsible Use of Control‑IQ Technology
Even with advanced systems such as the t:slim X2 insulin pump with Control-IQ technology, users are still responsible for actively managing their diabetes. Control-IQ technology does not prevent all high and low blood glucose events. The system is designed to help reduce glucose variability, but it requires that users accurately input information, such as meals and periods of sleep or exercise. Control-IQ technology will not function as intended unless all system components, including CGM, infusion sets and pump cartridges, are used as instructed. Importantly, the system cannot adjust insulin dosing if the pump is not receiving CGM readings. Because there are situations and emergencies that the system may not be capable of identifying or addressing, users should always pay attention to their symptoms and treat accordingly.
Important Safety Information
RX ONLY. The t:slim X2 pump and Control-IQ technology are intended for single patient use. The t:slim X2 pump and Control-IQ technology are indicated for use with U-100 insulin only. t:slim X2 insulin pump: The t:slim X2 insulin pump with interoperable technology is an alternate controller enabled (ACE) pump that is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in people requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The t:slim X2 pump is indicated for use in individuals six years of age and greater. Control-IQ technology: Control-IQ technology is intended for use with a compatible integrated continuous glucose monitor (iCGM, sold separately) and ACE pump to automatically increase, decrease, and suspend delivery of basal insulin based on iCGM readings and predicted glucose values. It can also deliver correction boluses when the glucose value is predicted to exceed a predefined threshold. Control-IQ technology is intended for the management of Type 1 diabetes mellitus in persons six years of age and greater.
Warning: Control-IQ technology should not be used by anyone under the age of six years old. It should also not be used in patients who require less than 10 units of insulin per day or who weigh less than 55 pounds.
Control-IQ technology is not indicated for use in pregnant women, people on dialysis, or critically ill patients. Do not use Control-IQ technology if using hydroxyurea. Users of the t:slim X2 pump and Control-IQ technology must: use the insulin pump, CGM, and all other system components in accordance with their respective instructions for use; test blood glucose levels as recommended by their healthcare provider; demonstrate adequate carb-counting skills; maintain sufficient diabetes self-care skills; see healthcare provider(s) regularly; and have adequate vision and/or hearing to recognize all functions of the pump, including alerts, alarms, and reminders. The t:slim X2 pump, and the CGM transmitter and sensor must be removed before MRI, CT, or diathermy treatment. Visit tandemdiabetes.com/safetyinfo for additional important safety information.