Medically reviewed by Dr. Jordan Pinsker, Vice President & Medical Director, Tandem Diabetes Care.
Kids love snacks! They are a great way to keep them content between meals. But for a child living with diabetes, it’s important to understand how those snacks impact blood glucose levels, while also making sure they can be properly matched with insulin.
Coming up with snack ideas for children living with diabetes can sometimes be tricky — particularly when pre-packaged, easy-to-grab snacks tend to have a lot of extra sugar and calories. Many parents struggle to come up with three square meals a day, let alone getting creative with snacks.
It’s common for families that have kids living with diabetes to get stuck in the same rotation when they find foods and portions that work for them. This article offers some fresh ideas that are a fun and healthy option for kids with diabetes.
Dr. Jordan Pinsker, the Vice President and Medical Director for Tandem Diabetes Care, who is also a leading pediatric endocrinologist, cautions parents that snacking and insulin management can vary from child to child based on several factors, including weight and age.
“The way I explain this to my adult patients is that for a low blood sugar, they should take 15 grams of carbohydrate, and then check their blood sugar in 15 minutes,” Dr. Pinsker said. “This is what’s known as the ‘Rule of 15.’ While this works for adults, this can be too much sugar for a small child, especially if they’re using an automated insulin delivery system.”

Snack Ideas for Children with Diabetes
Here’s a short guide to snack options for kids living with type 1 diabetes. Below, parents and caretakers will find several yummy snack ideas that will fit into an insulin resistance diet and are quick to throw together — better yet, require almost no prep work — along with must-know tips for helping children develop a healthy relationship with food.
Studies show that adolescents with type 1 diabetes are twice as likely to develop an eating disorder than individuals without diabetes, which makes it even more crucial to model and cultivate a positive attitude towards food.
Please keep in mind:
- These are not one-size-fits-all suggestions
- Serving sizes will depend on the child’s age, activity level, or treatment plan
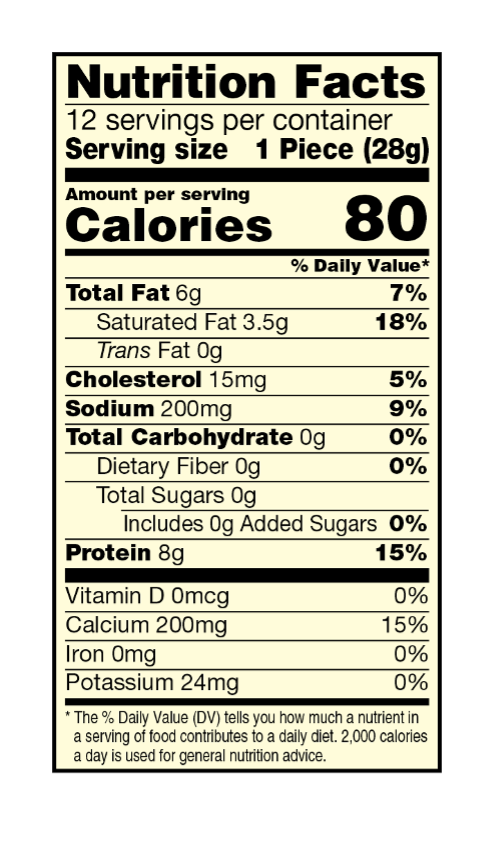
- Read the package portion size – here’s an example of what you’d see for a string cheese snack, a popular option for kids (this one is from Sargento)
“It can be difficult to differentiate between what’s nutritious while still trying to minimize carbohydrate intake,” Pinsker said. “For example, smoothies and breads can be nutritious, but they also have a lot of glucose, and it can be challenging to balance the insulin intake. It’s best to focus on foods with little or no carbohydrates.”
Note: Always consult with your child’s healthcare provider before making any significant changes to diet or type 1 diabetes management.
Now, let’s get to snacking!
Greek Yogurt with Toppings
Not all yogurt is created equal, but in general, plain Greek yogurt is a fantastic choice for people living with diabetes. Unflavored Greek yogurt has less sugar, and it’s also a great source of protein, fat, and probiotics for digestive health. Here are some ideas for toppings:
- PB2 powder, thoroughly mixed, to make peanut-butter-flavored yogurt
- Nuts and seeds
- Cinnamon
- Mixed berries (Be sure to calculate insulin for the berries)
Parent hack
Try adding a sugar substitute like stevia or agave nectar to sweeten it up.
“Ants on a Log”
This tried-and-true classic never goes out of style. Ants on a log packs a real punch when it comes to flavor and staying power. To make, spread peanut butter on a handful of celery sticks (the “logs”). Then, line raisins along each stick (the “ants”). This is a fiber-rich snack thanks to the celery, while the peanut butter makes it more satiating and tastier at the same time.
Parent hack
If you need to reduce the carbs or glucose levels, try using cream cheese instead of peanut butter and raisins.
Hummus with Veggies and Crackers
First-time makers are always shocked at how easy it is to whip up a fresh batch of hummus. Simply throw some garlic, chickpeas, olive oil, and lemon into a blender — and voila! — a protein- and iron-packed spread that’s perfect with baby carrots, celery, cucumbers, pita crackers, and whole grain toast. (Make sure to balance insulin accordingly for crackers or toast sticks.)
Parent hack
Veggies are a great low-carb option, but they add up. Keep in mind that a full cup of vegetables counts as a single serving of carbs.
Chia Seed Pudding
Chia seed pudding is a cross between overnight oats and rice pudding. To make, fill a jar with chia seeds and dairy or non-dairy milk and soak it overnight in the refrigerator. During the night, the seeds will begin to expand as they soak up the liquid, turning the concoction into a delicious, nutrient-dense treat. Tasty add-ons could include vanilla, nuts and seeds, cinnamon, or berries.
Parent hack
If you’re worried about the milk-to-carb ratio, try a nut-based milk.
On-the-Go Snack Ideas
Though it’s ideal to opt for homemade snacks over processed food items, life doesn’t always allow for it. And that’s okay. Some pre-packaged snacks (no prep necessary) include:
- Low-sugar fruit and nut bars
- String cheese
- Roasted nuts
- Air-popped popcorn
Parent hack
Homemade popcorn is healthier, but you’ll still have to account for the carbohydrates.
Additional Tips
When preparing a snack for multiple children, some of whom aren’t living with diabetes, aim to serve the same snack. Not only does this make it easier on the parent or caregiver, but it also prevents the child who’s living with diabetes from feeling like they’re being deprived in any way. This also helps create a positive relationship with food, since diabetes-friendly snacks are typically healthy for the whole family.
It’s also helpful to write the carbohydrate amount on the snack bag so that if the child is away from home, dosing for snacks becomes easier.
If possible, involve the child in prepping the snack. This is a wonderful practice for all children, not just those living with diabetes. But for a child who is living with diabetes, who may feel like they have no freedom over what and when they eat (especially compared to other kids they see), lending a hand or taking over their snack preparation can be empowering.
Snacks don’t need to be as balanced as meals, but it’s ideal to include more than a single component. For example, a well-balanced meal for a child with diabetes should include mostly non-starchy vegetables, some carbs, and some protein. A snack, on the other hand, doesn’t need all of that, but try to do a variation of:
- Fiber (fruit, veggie, or whole grain) + fat
- Fiber (fruit, veggie, or whole grain) + protein

Talking About Food to Kids with Type 1 Diabetes
Language is powerful, and how parents and children with diabetes communicate about food can have a lasting impact. Here are some ways to reframe “diet” when talking to children living with diabetes:
- Instead of, “You should eat this,” consider, “Eating these types of foods help your body feel strong.”
- Instead of, “That food is bad for you,” consider, “That would be a tasty treat. Let’s save that choice for a special occasion.”
- Instead of, “Eat whatever I serve you,” or, “Eat what’s on your plate,” consider, “This is what we are making today — you can choose between these two ‘growing foods.’” This last option allows young ones a bit of autonomy, even if the choice is between peas or green beans.
One More Note
It’s common for families impacted by diabetes to mourn the loss of spontaneity, especially when it comes to food and the joy associated with treats. But here’s the good news: While spontaneity may not be a frequent visitor, joy can very much be a permanent resident. Managing diabetes doesn’t have to be all about restriction. You can work with your diabetes educator to understand how to match insulin to the carbs in special treats like pizza or birthday cake.
Understanding the interplay between insulin and diet will allow room for the occasional treat. Work with a registered dietitian to gain more confidence in prepping meals and snacks, and set the foundation for a positive attitude towards eating and diabetes management.
Unless otherwise noted, all medical information was provided by Jordan Pinsker, MD, and Molly McElwee Malloy, RN, CDCES of Tandem Diabetes Care, Inc.